Journal of Current Emergency Medicine Reports
Burden on Healthcare Professionals in a Tertiary Care Hospital in the State Capital of the Indian Subcontinent
Surjeet Acharya1*![]() , Aisvarya Kapoor2, and Kishalay Datta3
, Aisvarya Kapoor2, and Kishalay Datta3
1Post Graduate trainee, Emergency Medicine, Max Super speciality Hospital, Shalimar Bagh, Delhi, India
2Consultant, Emergency Medicine, Max Super Speciality Hospital, Shalimar Bagh, Delhi, India
3Director and HOD, Emergency Medicine, Max Super Speciality Hospital, Shalimar Bagh, Delhi, India
*Corresponding Author: Acharya S, Emergency Medicine Resident, Department of Emergency Medicine Max Hospital, Shalimar Bagh, New Delhi, India. E-mail: drsa2495@gmail.com
Citation: Acharya S, Kapoor A, Datta K. Factors Influencing People to Leave Against Medical Advice in A Tertiary Care Centre in New Delhi, India. Journal of Current Emergency Medicine Reports. 2021;1(2):1-9.
Copyright: © 2021 Acharya S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received on: 8th September, 2021 Accepted on: 1st October, 2021 Published on: 10th October, 2021
Abstract
Healthcare and related professions have been identified as occupations associated with high levels of risk and stress. This has brought hazardous impacts not only on healthcare professionals’ mental and physical health but also on their abilities to cope with rising demands on the job. There are many reports of violence against doctors, which can sometimes be grievous and also fatal all across the world and also from our Indian subcontinent too. In this study article, we focus on whether the healthcare professionals in a tertiary care hospital in Delhi feel safe in their workplace, the burden they face on the work front and the knowledge of healthcare professionals about the Indian Epidemic Act Ordinance 2020. We also highlight the work-related stress that is faced by all healthcare professionals.
Keywords: Occupational stress, physical stress, emotional stress, Indian Epidemic Ordinance act 2020, abusive patients and attendants, abuse on healthcare professionals
Abbreviations
- ER – emergency room
- ICU – intensive care units
- Fig – figure
- IED 2020 – Indian Epidemic Disease (Amendment)
- MPA – Medical Protection Act
- IPC – Indian Penal Code
- CrPC – Code of Criminal procedure
Introduction
India is a developing nation with the second largest population in the world and healthcare system in India still growing. This has recently become a keen interest among social media in India to notice how the healthcare personnel are manhandled and ill-treated. The covid-19 scenario has highlighted many major loopholes in the healthcare system including unsafe practising environment even during pandemic. In this study, we will try to find out and list down how frequently medical personnel or hospital staff (from doctors to security to the administration) are ill-treated and manhandled. We will also elaborate how the ill-treatment from the patients and attendants affects the mental health of healthcare workers and the levels of stress endured by them and the ways out to reduce stress.
Review of Literature
Violence against healthcare professionals or other medical fraternity hardly made any news or was hardly discussed about a few years back in India. In studies conducted and analysed, in majority of the cases (60-70%) violence was in the form of either aggressive gesture or verbal abuse [1,2,3,4,5]. Often, these people who abused a medical professional were themselves under the influence of substance abuse or were in the psychiatric wards [6]. In the western world, areas of high-risk have been identified as waiting areas of the Emergency room, Intensive Care Units (ICU) [6,7,8]. Often in the Indian subcontinent, patients by themselves are not the only violence makers but also their relatives, political leaders and political parties misuse their powers and take the law into their hands [2,3]. India has the second largest population in the world and the healthcare sector is a growing field. Various studies have shown that senior healthcare professionals whether be a doctor or nurse, are less likely to face any type of abuse from a patient or attendant as compared to their junior colleagues [2,5].
Another problem faced by healthcare professionals in India along with occupation risk is work related stress. Stress is a multidimensional concept. The word stress arises from the Latin word “stringere” which means to describe hardship/afflictions. Work stress among healthcare professionals can have negative outcomes like job burnout, alcohol/ substance/tobacco dependency, adverse psychological well-being and larger number of suicides attempts as well as other psychological, social and emotional problems [10]. Various studies conducted to identify the culprits of stress in healthcare providers (for each category) showed that the main sources of stress were excessive workload, underpayment, inadequate staffing, and being involved in the emotional distress of patients [10]. Stress also harms professional effectiveness: reduces concentration [12], reduces providers’ abilities to establish strong relationships with patients [13], it decreases attention [14], impinges on decision-making skills [15], and also leads to excessive burnout and has been defined as a syndrome of emotional exhaustion, depersonalization and a sense of low personal accomplishment [16].
Material and Methods
The study was done in a tertiary care corporate hospital in New Delhi.
Inclusion criteria:
- People willing to participate
- All the healthcare workers working in the hospital (Max Super speciality hospital, Shalimar Bagh, New) dealing with patients / attendants directly
- Exclusion criteria
- People not consenting for the study / participation
The study questionnaire is developed after detailed review of studies done in similar settings [2,4,6,17,18]. All the data was collected from healthcare personnel (doctor, nurse and allied staff). A structured questionnaire was made and given to participants for recording their responses online or in person.
Results
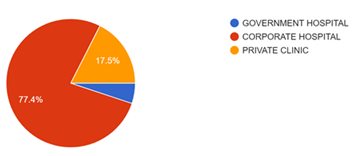
We got a good response from our hospital staff including those working in ER, ICU and wards as well as few from private clinic practice (Figure 1). The total number of participants who participated in this study and completed the full questionnaire were 157.
Major contributions were from corporate hospitals followed by private clinics. A very few contributions were from government hospital personnel.
Figure 1: Total number of participants who participated in this study.
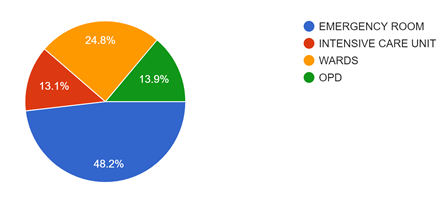
Figure 2: Describes the study population which were involved from various departments of our hospital. Being an emergency doctor, we have received a good response from the ER when compared to other areas of the hospital.
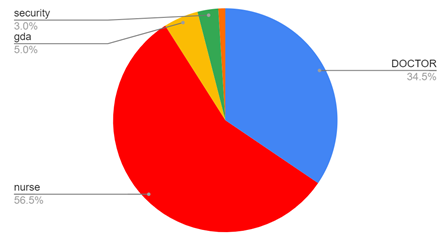
Figure 3: Describes the contribution of respective individuals participating in the study. Most contribution was done by the nursing staff followed by doctors and rest contribution as per pie chart given below.
Figure 4: Describes the gender of the participants. Females were most in number to respond to this survey.
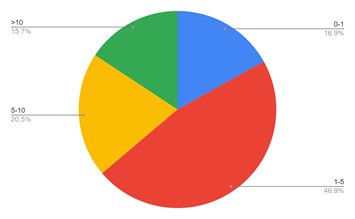
Figure 5: Shows the experience of the participants involved in the study. The experience of the patients were majorly around 1-5 years and very few were in seniority (>10 years of experience).
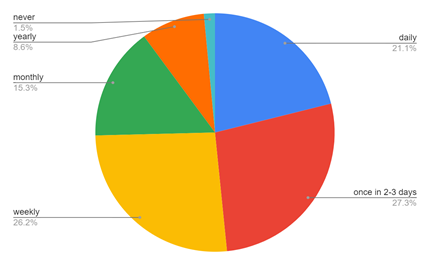
Figure 6: Shows the major part of this study. It describes how often the medical fraternity gets exposed to improper behaviour by the patient/attendant.
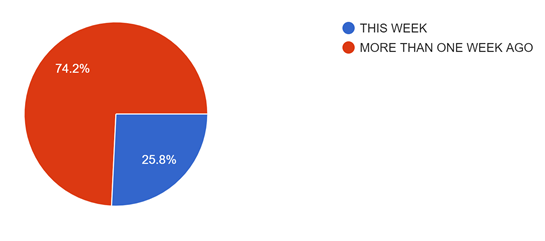
Figure 7: Shows how recently the participants were exposed to abuse by the patient/attendant. Majority of the people have encountered an abusive patient or attendant within a week of this study.
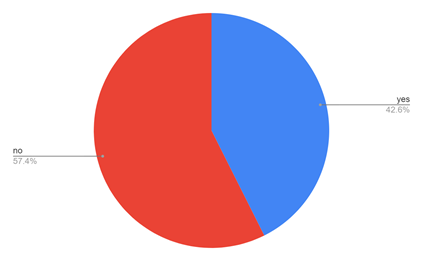
Figure 8: Shows how often the healthcare worker feels threatened at the workplace. Around 43% (approximately) of the healthcare workers feel threatened at the workplace. Approximately 57% of people don’t feel threatened at the workplace due to the security and other protective measures practised in big hospitals.
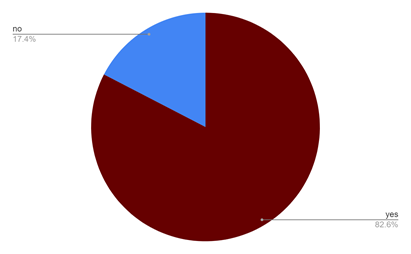
Figure 9: Shows the involvement (or supports) of seniors in situations where the participants get abused by patients/attendants. It has been seen that a senior team member is always more listened to and handles the situation better when compared to the younger colleagues.
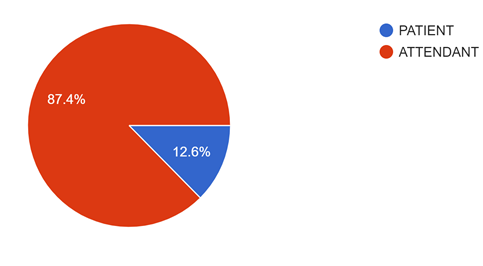
Figure 10: Shows the involvement of either patient or attendant during the abusive act. The majority is done by the attendants.
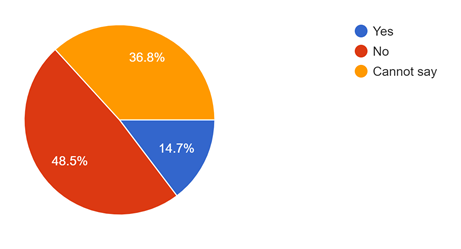
Figure 11: Shows if the patient or attendant was under the influence of alcohol or any other substance abuse during the act of abusive episode.
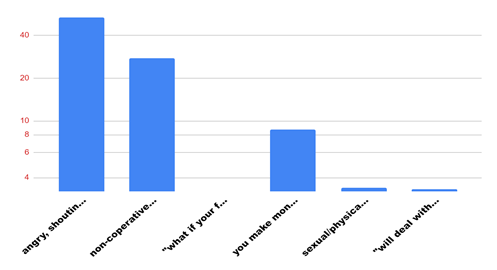
Majority of the participants responded that they have faced angry/shouting and verbal abuse from patients/attendants. The next was non-cooperation from the patients/attendants. Next abuse faced by healthcare professionals is that the healthcare professionals make unwanted money from them. Threatening to face dire consequences later on is next abuse hurled at healthcare professionals.
Figure 12: Shows the bar graph showing the most common abuses (physical/sexual/verbal).
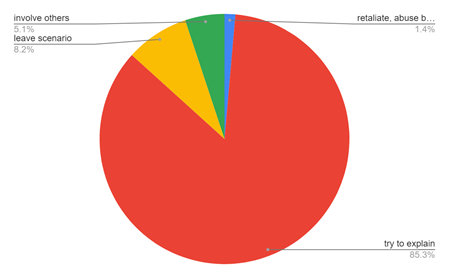
Figure 13: Shows how the healthcare workers react to any abusive environment. Most common reaction of healthcare workers is to try to explain to them the situation/scenario and help them out.
Figure 14: Describes how often healthcare workers want to quit their profession. The largest portion is by healthcare staff who want to quit the profession whenever they face such situations but later change their mind.
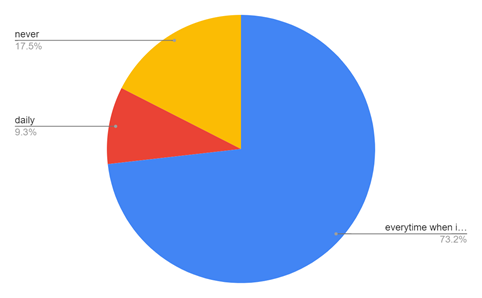
Figure 15: Demonstrates how the study participants try to manage between the professional environment and personal life.
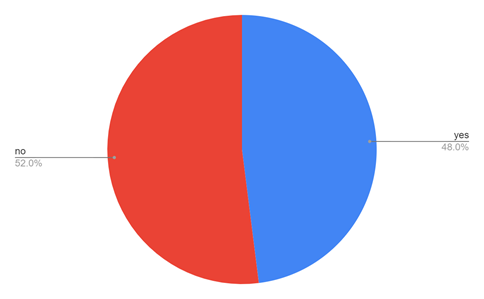
Figure 16 explains whether the professional life of healthcare workers affects their personal life. Though less in number, the majority of healthcare workers’ personal life is affected by their professional life.
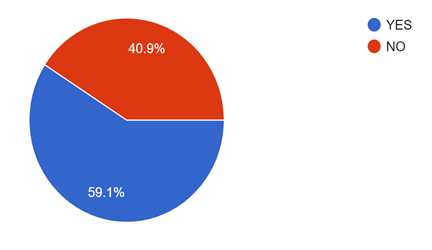
Figure 17 shows how well informed are the healthcare workers about the epidemic act ordinance passed in 2020 for protection of healthcare workers. Sadly, around 40 % of the healthcare workers still don’t know about this ordinance.
Discussion
“No physician, however conscientious or careful, can tell what day or hour he may not be the object of some undeserved attack, malicious accusation, black mail or suit for damages….’ [11]
The above line is from a reputed Journal from the USA, written 135 years ago and should be an eye-opener and also prophetic.
Common public perception is that the majority of the medical fraternity (especially in private or corporate hospitals) make patients undergo unnecessary testing / treatment / procedures and this is a major cause of disagreement leading to conflict from the patient side. Majority of the hospitals in India lack any proper grievance redressal system. Also, legal procedures in India also take inordinately long time. So, the steps to prevent such attacks on medical professionals can be prevented by working at various individual levels as below:
Healthcare professional level
The professionals must train himself/herself for anxiety alleviation techniques, reduce waiting hours to see patients, explain the condition of the patient to the attendant individually to avoid any conflict at later stages, keep in mind the financial status of the patients, and take help from seniors whenever needed.
Hospital level
(i) There should be a proper grievance redressal system in the hospital
(ii) There should be complete transparency on costs of different investigations and treatment, rents and other expenses in the hospital with no hidden charges
(iii) Adequate number of medical staff to ease the rush of patients and long waiting hours;
(iv) Hospital security should be strengthened and must work in close relation with nearby police station
(v) Use of computer and internet technology to facilitate documentation related to waiting time.
Media level
Both print and electronic media must understand that medicine in not definitive and no diseases are 100 percent curable. With use of knowledge, new evidence and new investigations, healthcare professionals try to help the community. Media must not sensationalize such instances for their TRP and augment the public anxiety or mistrust in the healthcare system.
Government and Political parties’ level
It is the major role of the government and the political parties as well as the policy makers to see that there is a big difference between the ever-growing Indian population and the number of doctors and medical staff. Instead of criticizing the medical fraternity, political parties and policy makers must act on “preventive medicine”. It is a very difficult task to build hospital beds for every individual in this country, so prevention of disease is the way to reduce the number of sick patients in the community. Also, there must be firm actions against the law breakers who are becoming part of such violence against doctors.
Patient level
Becoming violent against medical professionals is not a part of modern civilised society. Patients and attendants must understand that medicine is not black and white and not all diseases are 100 % curable. A sense of trust must be developed for their treating doctor and his team to get fruitful results. In our study, we have seen that the attendants were more common people causing the nuisance than the patient themselves.
Most of the violent activities go under reported. This is because, many considered it as an useless and time-wasting activity. This shows the need to encourage reporting of such violence among healthcare workers and to develop institutional strategies for speedy measures to avoid such drastic events. In our study, it is seen that many professionals were exposed to such violent and abusive patients within the recent past.
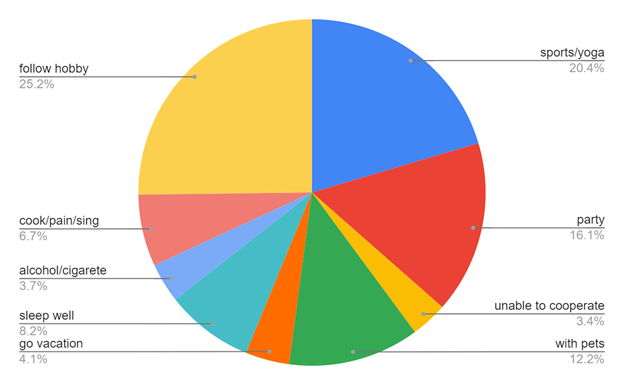
There is also a significant number of healthcare professionals experiencing workplace stress. Our study has shown a significant number of professionals suffering from work related stress which also affects their personal life also. Workload and working in night shifts were the most common source associated with workplace stress. Our study has shown various activities taken up by professionals to reduce the work-related stress or hardship seen by them at the workplace. This professional stress sometimes also provokes the healthcare professionals to quit the healthcare sector. Health policy makers and hospital managers should identify such sources and should be concerned about workplace stress.
For the protection of healthcare professionals, the government of India has passed an ordinance which sadly remains unknown by many. If known, the ordinance is not practised by many. It is the “INDIAN EPIDEMIC DISEASE (AMENDMENT) ORDINANCE 2020” and “MEDICAL PROTECTION ACT”. The IED amendment ordinance 2020 was promulgated on April 22, 2020. The Ordinance amends the Epidemic Diseases Act, 1897. The Act provides for the prevention of the spread of dangerous epidemic diseases. The Ordinance amends the Act to include protections for healthcare personnel combatting epidemic diseases and expands the powers of the central government to prevent the spread of such diseases.
Key features of the ordinance include:
- An ‘act of violence’ includes any of the following acts committed against a healthcare service personnel: (i) harassment impacting living or working conditions, (ii) harm, injury, hurt, or danger to life, (iii) obstruction in discharge of his duties, and (iv) loss or damage to the property or documents of the healthcare service personnel.
- The Ordinance specifies that no person can: (i) commit or abet the commission of an act of violence against a healthcare service personnel, or (ii) abet or cause damage or loss to any property during an epidemic. Contravention of this provision is punishable with imprisonment between three months and five years, and a fine between Rs 50,000 and two lakh rupees. This offence may be compounded by the victim with the permission of the Court. If an act of violence against a healthcare service personnel causes grievous harm, the person committing the offence will be punishable with imprisonment between six months and seven years, and a fine between one lakh rupees and five lakh rupees. These offences are cognizable and non-bailable.
- Persons convicted of offences under the Ordinance will also be liable to pay compensation to the healthcare service personnel whom they have hurt. Such compensation will be determined by the Court. In the case of damage or loss of property, the compensation payable to the victim will be twice the amount of the fair market value of the damaged or lost property, as determined by the Court. If the convicted person fails to pay the compensation, the amount will be recovered as an arrear of land revenue under the Revenue Recovery Act, 1890.
- Investigation: Cases registered under the Ordinance will be investigated by a police officer not below the rank of Inspector. The investigation must be completed within 30 days from the date of registration of the First Information Report.
- Trial: The inquiry or trial should be concluded within one year. If it is not concluded within this time period, the Judge must record the reasons for the delay and extend the time period. However, the time period may not be extended for more than six months at a time.
The MPA instead, protects doctors from any crime against them. But unfortunately, it is not listed in the IPC (Indian penal code) and the CrPC (code of criminal procedure). Thus, the victim cannot proceed with court or police regarding any lawful action done against him/her. Offenders can get a jail term of up to three years and a fine of Rs 50,000.
We need more studies to see the actual state of healthcare professionals and how they deal with day-to-day stress in their profession. A larger group study will highlight more on these issues and will tell us about the awareness of above acts in medical professionals. We also need more stringent laws to protect the medical staff not only during epidemics or pandemic but also on a daily basis. Results from such studies will help the policy makers and government to frame proper guidelines and rules and regulation for healthcare professionals’ safety and to ease the burden on the Indian healthcare structure.
Conclusion
The study done in the tertiary care setup included healthcare professionals from all the departments. Study was limited by the study population as very few participants completed the whole study questionnaire. The results of the study showed that young, female, healthcare professionals were most in number on the receiving spectrum of verbal abusive patients. Patient attendants were most commonly involved in creating a non-functional environment in the healthcare setup. The work-related stress among the healthcare professionals is very high leading to imbalance between their professional and personal life and increasing their mental stress.
Acknowledgement
I/we certify that I/we have participated sufficiently in the intellectual content, conception and design of this work or the analysis and interpretation of the data (when applicable), as well as the writing of the manuscript, to take public responsibility for it and have agreed to have my/our name listed as a contributor. I/we believe the manuscript represents valid work. Neither this manuscript nor one with substantially similar content under my/our authorship has been published or is being considered for publication elsewhere, except as described in the covering letter. I/we certify that all the data collected during the study is presented in this manuscript and no data from the study has been or will be published separately. I/we attest that, if requested by the editors, I/we will provide the data/information or will cooperate fully in obtaining and providing the data/information on which the manuscript is based, for examination by the editors or their assignees. Financial interests, direct or indirect, that exist or may be perceived to exist for individual contributors in connection with the content of this paper have been disclosed in the cover letter. Sources of outside support of the project are named in the cover letter. I/We hereby transfer(s), assign(s), or otherwise convey(s) all copyright ownership, including any and all rights incidental thereto, exclusively to this journal, in the event that such work is published by this journal. The Journal shall own the work, including copyright; the right to grant permission to republish the article in whole or in part, with or without fee; the right to produce preprints or reprints and translate into languages other than English for sale or free distribution; and the right to republish the work in a collection of articles in any other mechanical or electronic format. We give the rights to the corresponding author to make necessary changes as per the request of the journal, do the rest of the correspondence on our behalf and he/she will act as the guarantor for the manuscript on our behalf. All persons who have made substantial contributions to the work reported in the manuscript, but who are not contributors, are named in the Acknowledgement and have given me/us their written permission to be named. If I/we do not include an Acknowledgement that means I/we have not received substantial contributions from non-contributors and no contributor has been omitted.
References
- Xianyu Y, Lambert VA. Investigation of the relationships among workplace stressors, ways of coping, and the mental health of Chinese head nurses. Nursing & health sciences. 2006 Sep;8(3):147-55.
- Phillips JP. Workplace violence against health care workers in the United States. New England journal of medicine. 2016 Apr 28;374(17):1661-9.
- Peng W, Ding G, Tang Q, Xu L. Continuing violence against medical personnel in China: A flagrant violation of Chinese law. Bioscience trends. 2016;10(3):240-3.
- Ambesh P. Violence against doctors in the Indian subcontinent: A rising bane. Indian heart journal. 2016 Sep 1;68(5):749-50.
- Anand T, Grover S, Kumar R, Kumar M, Ingle GK. Workplace violence against resident doctors in a tertiary care hospital in Delhi. The National medical journal of India. 2016 Nov 1;29(6):344.
- Ferri P, Silvestri M, Artoni C, Di Lorenzo R. Workplace violence in different settings and among various health professionals in an Italian general hospital: a cross-sectional study. Psychology research and behavior management. 2016; 9:263.
- Ifediora C. Exploring the safety measures by doctors on after-hours house call services. The Australasian medical journal. 2015;8(7):239.
- http://www.timesofindia.indiatimes.com/india/Over-75-of-doctors-have-faced-violence-at-work-study-finds/articleshow/47143806.cms .
- Gregov L, Kovačević A, Slišković A. Stress among Croatian physicians: comparison between physicians working in emergency medical service and health centers: pilot study. Croatian medical journal. 2011 Feb 15;52(1):8-15.
- Saha D, Sinha R, Bhavsar K. Understanding job stress among healthcare staff. Online Journal of Health and Allied Sciences. 2011 Apr 15;10(1).
- Assaults upon medical men. Journal of the American Medical Association. 1892; 18:399–400.
- Bower JE, Segerstrom SC. Stress management, finding benefit, and immune function: positive mechanisms for intervention effects on physiology. Journal of psychosomatic research. 2004 Jan 1;56(1):9-11.
- McGonagle KA, Kessler RC. Chronic stress, acute stress, and depressive symptoms. American journal of community psychology. 1990 Oct;18(5):681-706.
- Emmett S. Why lawyers need resilience. Bulletin (Law Society of South Australia). 2013 Apr;35(3):31.
- Linden W, Lenz JW, Con AH. Individualized stress management for primary hypertension: a randomized trial. Archives of internal medicine. 2001 Apr 23;161(8):1071-80.
- Tamini BK, Kord B. Burnout components as predictors of job & life satisfaction of university employees. Indian Journal of Industrial Relations. 2011 Jul 1:126-37.
- https://www.huffpost.com/archive/in/entry/ek-doctor-ki-maut-india-a_b_7288100
- Kitaneh M, Hamdan M. Workplace violence against physicians and nurses in Palestinian public hospitals: a cross-sectional study. BMC health services research. 2012 Dec;12(1):1-9.